Equipped with one of the largest medicolegal claims databases in Canada, Health Insurance Reciprocal of Canada (HIROC) embarked on a plan
in 2011 to decode patient safety knowledge, as extracted from medical professional liability (MPL) claims, to inform leaders and practitioners within the healthcare system.
This included development of (1) a list of the top risks that had resulted
in the most costly claims for acute-care organizations (ACOs), (2) concise reference sheets for each risk, highlighting claims findings, themes,
case studies, and key mitigation strategies, and (3) the Risk Assessment Checklists (RAC),
an online program that organizations can use to systematically self-assess compliance with the top 10 evidence-based mitigation strategies for each risk. As challenging as risk identification can be, risk assessment (the determination of how bad or how often a risk may occur) is even more so but is nevertheless essential to the process of prioritization of these strategies.
Medicolegal claims can be used to identify important and actionable deficiencies in health- care processes that are not generally captured by other data sources (Levtzion-Korach et al.,
2010). Claim files provide qualitative information that can be used to analyze adverse events, and to identify latent and systemic issues (Vincent et al., 2006; Thomas & Petersen, 2003). Analysis of aggregated claims data in anesthesiology, for example, led to the creation of professional standards requiring pulse oximetry and end-tidal carbon dioxide monitoring in the operating room, which dramatically decreased associated risks (Vincent et al., 2006).
2020 Top risks for Canadian acute-care organizations
Since 2011, the list of the top risks leading to the most costly claims has been updated every three years to reflect new and evolving risks in healthcare. The methodology for the 2020 ranking varied from prior years: Only claims with total incurred claims costs of greater than $500,000 (Canadian) were included. In general, claims costs over this threshold are more likely to be pursued and often contain two or more nonsuppurative peer expert reports. A preliminary analysis by HIROC suggests that the 2020 top 10 claims sources for acute-care hospitals will be the following:
1. Maternal/Neonate: Failure to interpret/respond to abnormal fetal status (during labor)
2. Maternal/Neonate: Mismanagement of induction/augmentation medications
3. Medical/Surgical: Failure to appreciate status changes/deteriorating patient
4. Mental Health: In-patient suicide/self-harm
5. Maternal/Neonate: Neonatal hyperbilirubinemia
6. Infections: Healthcare acquired infections
7. Maternal/Neonate: Neonatal hypoglycemia
8. Medication: Medication adverse events
9. Maternal/Neonate: Delayed/access issues C-sections
10. Falls: Falls—patients.
These 10 risks fall into five general areas or themes: maternal/neonatal-related risks, patient deterioration, on-premise suicide/self-harm, healthcare- acquired infections, and falls.
Maternal/neonatal-related risks
Birth trauma to the newborn or fetus can signal significant life- altering harm for newborns and families, requiring long-term care and treatment. Multifaceted evidence-informed obstetrical quality improvement programs have been identified as one of the most promising interventions for reducing harm and medical professional liability claims. It is estimated that one in every 1,000 births are reported to HIROC by its subscribers, with more than 60% of those infants experiencing a major or catastrophic outcome. Discouragingly, the most common contributing factors associated with such matters have remained relatively constant over the last two decades, and birth trauma and injury remain among the most serious safety challenges for hospitals. The top two risk themes—interpretation and response to abnormal fetal status and management of induction/ augmentation medication (IV oxytocin)—contribute to more than 35% of all claims costs. Two of the neonatal themes— hyperbilirubinemia and hypo- glycemia—have been identified as highly preventable metabolic disorders on the Canadian Patient Safety Institute’s “never events” list (2014).
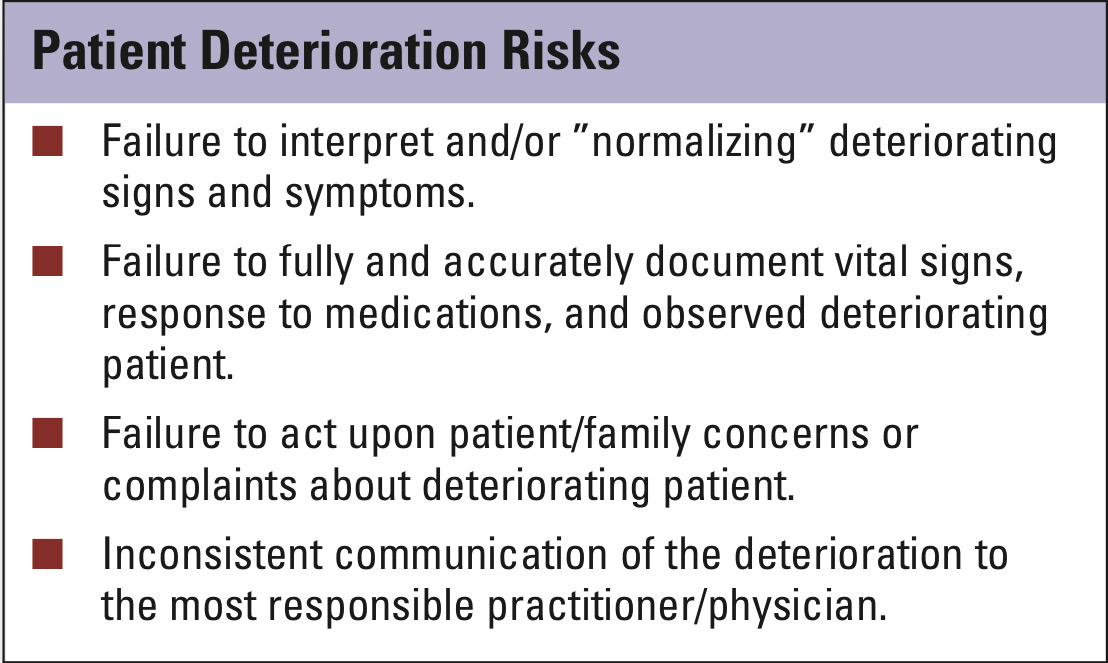
Patient deterioration
For 2020, “failure to appreciate status changes/deteriorating patient” (also known as the failure-to-res- cue) has dropped from the second
to the third priority position on the list. As evidenced from HIROC claims and the medical literature, the positive impact of early identification and management of patient deterioration on clinical outcomes is well documented. Family members often notice changes in the patient’s alertness and level of awareness as well as in restlessness or agitation. Deterioration may not be recognized or acted upon by healthcare providers (HCPs) resulting in preventable patient safety incidents. Early identification and, as warranted, escalation of care concerns by families and clinicians are key to managing this risk.
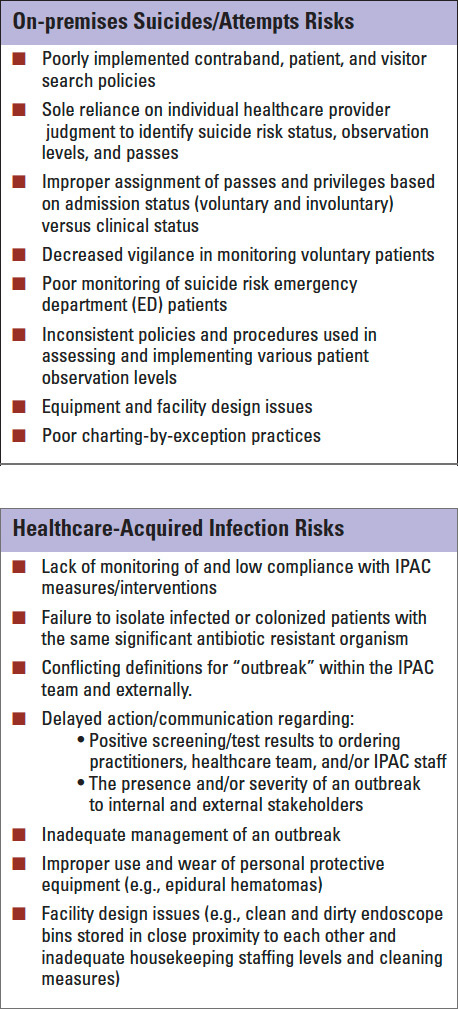
On-premise suicides/self-harm
A troubling trend is on-premises suicides. This includes suicide “attempts,” in which the at-risk individual survived the attempt but nonetheless sustained permanent physical (e.g., paralysis or quadriplegia) and, often, neurological (e.g., asphyxia) sequalae. The high claims costs associated with such attempts reflect the ongoing and future care costs associated with the clinical outcome. Despite poor predictability, a number of clinical, procedural, and facility design factors have been identified as common, contributing, and avoidable.
Healthcare-acquired infections
Acquired during the delivery of healthcare (also known as nosocomial infection), healthcare acquired infection (HAI) claims remain a significant patient safety issue. There are multiple factors increasing the risk of HAIs, such as host factors (e.g., advanced age or underlying immunosuppression) complex treatment modalities, length of procedures, length of stay, and an increasing prevalence of antibiotic-resistant organisms. HIROC legal claims suggest that a breach of infection prevention and control (IPAC) practices that occurred around the time of the infection has contributed to the transmission of such infections.
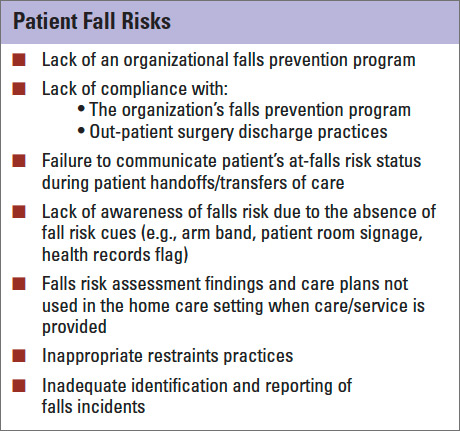
Falls
Patient falls is the last general theme of HIROC’s top risk areas. Defined as an inadvertent event that results in a person coming to rest on the ground or floor or other lower level (World Health Organization, 2018), injuries caused by falls frequently result in prolonged hospitalization and significant disabilities, with loss of independence, and associated costs. Some epidemiologic studies have found that falls occur at a rate of three to five per 1,000 bed days. While multifaceted strategies have been suggested to mitigate the risks of falls, it is unlikely that all falls and related harm can be prevented.