Informed consent requires that a patient understand the risks, benefits, and alternatives of a medical procedure. This process is crucial for patient-centered care and for fulfilling medical practitioners' ethical and legal obligations. However, it remains a significant liability concern for surgeons, and malpractice data can pinpoint where targeted improvements are most needed.
An adequate informed consent process involves a detailed discussion about the procedure between the patient and the provider, which emphasizes the patient’s role in the decision, sets realistic expectations regarding the outcomes, and secures formal consent if the patient chooses to proceed.
However, even after communicating all the necessary information, patients may not fully grasp the risks, benefits, and alternatives or have realistic expectations. Surgeons often worry about correctly providing and documenting the essential aspects of the informed consent process to comply with regulations, reduce liability, and protect their patients.
To help address these concerns, a team of CRICO and Candello analysts examined more than 9,500 surgery cases that closed between 2017 and 2021. Candello, a division of CRICO—the captive medical malpractice insurer for the Harvard medical community—manages a national database of open and closed malpractice claims provided by medical professional liability (MPL) insurers nationwide, including cases from a wide variety of hospitals. The goal was to gather insights into how informed consent contributes to malpractice cases, the factors affecting the odds of cases closing with an indemnity payment, and identify key areas of risk related to informed consent that can be mitigated.
Key Findings
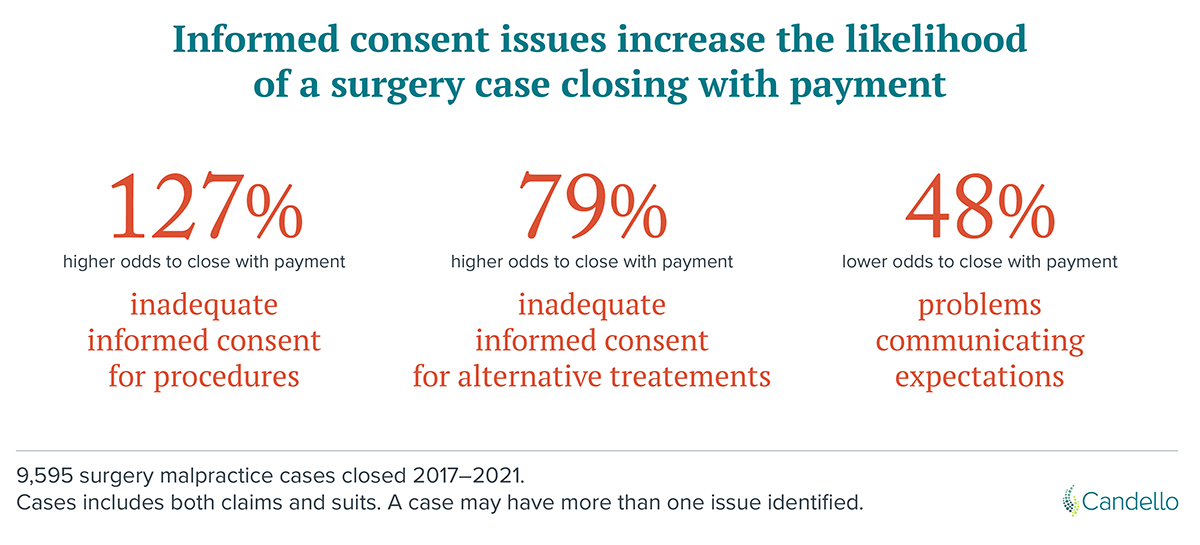
- Inadequate informed consent makes indemnity payment on a surgery malpractice claim more likely.
- The failure to discuss nonsurgical alternatives increases the likelihood of payment.
- Expectation management is important for avoiding claims, given its frequency, even though it is not a factor that increases the odds of a case closing with an indemnity payment.
The team identified three factors involving informed consent that can contribute to surgery claims.
1. Inadequate Informed Consent for Surgical or Invasive Procedures
For cases involving inadequate informed consent for a procedure, 49% resulted in an indemnity payment, with an average amount of $415,000. Many elements are needed to ensure a patient can comprehend and consent to a procedure, which creates multiple vulnerabilities in the process.
The Joint Commission’s publication, “Informed Consent: More Than Getting a Signature,” discusses barriers to understanding the procedure, such as a lack of basic information on the consent form, forms that do not incorporate health literacy principles and cultural differences across patient populations, and ineffective provider-patient communication.
2. Inadequate Discussion of Alternative Treatments
The analysis showed that insufficient discussion of alternatives to surgery or invasive procedures can be just as detrimental as inadequate informed consent to procedures. Of the surgery cases with inadequate discussion of alternative treatment options as part of the informed consent process, 50% closed with an indemnity payment, at an average of $400,000.
3. Problems with Communicating Expectations of Procedure Outcomes and Experiences
Problems communicating expectations were the most common informed consent factor among surgery cases. However, only 21% of these cases closed with payment, and these cases had the lowest average payment of the three factors--$309,000.

If a claim investigation finds a patient had unrealistic expectations about a treatment outcome, the patient may be less likely to receive compensation, depending on the other circumstances. Effectively setting realistic outcome expectations with a patient is integral to the informed consent process and could reduce the risk of a claim being asserted in the first place, even though this factor is associated with a relatively low likelihood of a claim closing with payment.
[Insert Graphic Here]
*Results are based on a multivariate analysis that also controlled for cases with high clinical severity (including death).
*Results are based on a multivariate analysis that also controlled for cases with high clinical severity (including death).
Other Considerations
Outside of the Candello analysis, other identified risk factors should be noted: A 2019 study in the Journal of Orthopedic Surgery—Hong Kong—assessed the informed consent process in elective versus trauma orthopedic surgeries. Trauma patients were found to have a significantly lower understanding of the proposed procedure, with key vulnerabilities in understanding possible complications and post-op care and expectations. Elective surgery patients had the lowest quality of understanding when it came to alternative treatment options.
Research conducted by Timothy Bhattacharyya and team also suggests conducting the informed consent process in the office compared to in the preoperative holding area may reduce the likelihood of a case closing with payment. Thoroughly describing the discussion of risks and benefits in a note in the medical record, in addition to the signed consent form, may also prevent financial losses.
Innovating Informed Consent
Innovations in the informed consent process are continuously sought as this critical aspect of care remains a significant risk to patient safety and malpractice.
Video-assisted consent methods are at the cutting edge of informed consent technology. Multiple clinical trials, including interventions for cataract surgery and trauma surgery, have shown that using educational videos in the process can improve a patient’s comprehension of provided information compared to only being given a consent form.
A 2020 systematic review of informed consent interventions published in Medical Decision Making also found that “teach-back” and interactive digital resources improved patient comprehension compared to multicomponent, audiovisual, or written interventions.
The cost for a video-assisted intervention may also not be as daunting as expected. Many materials, such as the examples below, already exist. Creating such resources could be an opportunity for cross-institutional collaboration to develop the resources and optimize their informed consent process.
The Candello analysis and other research show that informed consent issues still play a significant role in patient safety and MPL risk. Addressing these issues through improved communication, better documentation, and innovative technologies like video-assisted consent may be effective methods to mitigate vulnerabilities in the informed consent process and enhance patient safety.