The electronic healthcare records (EHR) revolution rests on a simple premise: connecting physicians, patients, and hospitals means higher quality and safer care. However, the marriage between technology and patient records remains rocky at best, beset by bugs that range from merely annoying to fatal.
Although electronic health records are rarely the primary cause of medical liability claims, they are increasingly cited as secondary claims contributing to patient injury, according to a study published by The Doctor’s Company.
The near-universal ubiquity of electronic healthcare records was prompted by the Health Information Technology for Economic and Clinical Health (HITECH) Act, passed by Congress and signed by then-President Barack Obama in 2009. In proposing this legislation a mere four weeks after his inauguration, Obama proclaimed,“We will make sure that every doctor’s office and hospital in this country is using cutting- edge technology and electronic medical records so that we can cut red tape, prevent medical mistakes and help save billions of dollars each year.”
Part of economic stimulus legislation designed to jump-start the economy, HITECH offered financial incentives for healthcare organizations and providers to adopt electronic healthcare records. Predictably, legislation unleashed a technological gold rush toward applying technology to the task of automating patient records.
In the decade since the passage of HITECH, a number of major electronic health record companies have emerged, promising to deliver on Obama’s pledge. To receive the incentives offered, hospitals, health organizations, and providers have stampeded into electronic medical records. The reality that they’ve run into reveals a sobering picture of the potential pitfalls of technology when applied to patient records.
EHR reality check
In an article entitled Electronic Health Records Continue to Lead to Medical Malpractice Suits, The Doctors Company noted that mistakes that are merely irritating with software features like the dropdown menu for selecting a specific state can become dangerous, or even lethal, when they precipitate an error in medication dosage or some other treatment.
In one case cited in the TDC report, a physician had to choose between one of two options in a dropdown menu—and selected the wrong one. The patient, upon filling his doctor’s prescription, got 200 mg of morphine sulfate instead of the intended 15mg. He ended up in the ER, and subsequently sued the doctor for causing emotional trauma, plus the costs of the ER treatment and hospital stay.
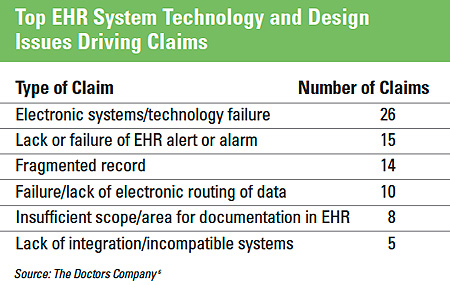
In its report, TDC analyzed the sources of EHR-related risks. The heterogeneous “other” category accounted for the highest claim count (30 claims), but other, specific issues were responsible for substantial numbers of suits, including electronic system failure, technology failure, and fragmented records.
A June 2019 study, by Mark Graber et al., published in the Journal
of Patient Safety, reached the conclusion that health information technology has improved“ the quality, safety, and efficiency of healthcare.” The article observed that “there is evidence that the number of malpractice suits has decreased in relation to the implementation of EHRs.”
The Graber article also acknowledged the significant flaws in current EHRs, including “limited interoperability, challenging user inter- faces, and software design that can degrade efficient clinician workflow.”
So, how did we get from the early promise of EHRs to this latter- day situation, wherein a tower of Babel cacophony seems to block, rather than enable, the exchange of patient information, and too many software features have evidenced an alarming tendency to degrade into potentially toxic bugs?
EHRs: The early days
A number of studies published in the early years of EHR adoption more often than not told of a positive relationship between the electronic storage of patient data and liability claims.
In one analysis, survey responses on medical professional liability (MPL) claims for the year 2005 were compiled on 1,140 practicing physicians. The results were scrutinized according to two factors: whether the doctors had adopted EHRs, and the presence or absence of MPL claims.
The study, published in the November 2008 Archives of Internal Medicine, found that 6.1% of physicians with EHRs, versus 10.8%
of physicians without them, had had paid MPL settlements within the last 10 years.
Tantalizingly, a secondary analysis found that 5.7% of “more active users,” compared with 12.1% of “less active users,” had paid settlements. On this basis, the authors speculated that “The federal government could also decide to offer subsidies for EHR adoption.”
But then a study published five years later on the relation between EHRs and MPL (Journal of General Internal Medicine, May 2013) reported that electronic records had, if anything, minimal impact: “Colorado physicians using office-based EHRs did not have significantly different rates of liability claims than non-users.” And the authors also reported on a second analysis: “Nor were rates different for EHR users before and after EHR implementation.”
The upshot was the standard recommendation for “further research . . . across the larger population of physicians.”
Still, there were also reports suggesting that adoption of EHRs was linked with measurable improvements in some of the salient aspects of healthcare, which might be expected to lower the rate of MPL claims. C. Tanner et al. (March 2015, Applied Clinical Informatics), noted that “having an EHR was strongly empirically associated with the workflow, policy, communication and cultural practices recommended for safe patient care in ambulatory settings.” This benefit seemed to stem largely from the “complex interactions between tech- nology and other aspects of the environment related to human resources, workflow, policy, among others.”
There were, in addition, reports on notable benefits in how providers went about their work. One report, in 2008, found that 82% of EHR users enjoyed improved clinical decision making, 92% had seen improvement in communication with other providers and their patients, and 82% had observed a reduction in medication errors. (C.M. DesRoches et al., New England Journal of Medicine, July 2008).
The relation of man and machine was, apparently, sufficiently seamless that both provider and patient stood to profit from the interaction between the two.
Enter HITECH
Meanwhile, the software programs being sold for EHRs had been proliferating at a breakneck pace, largely in response to the most fundamental incentive for any sort of enterprise: money. The passage of the HITECH Act in February 2009 authorized a hefty chunk of the massive stimulus package for health information technology. The goal was to get hospitals and doctors to buy EHRs, and also to induce them to use them in a way that would drive better care—“meaningful use.”
But even the Director of the Office of the National Coordinator for Health Information Technology at the time, Farzad Mostashari, recognized that this goal was more than likely elusive. It was his opinion that a useful, interoperable, nationwide records system was “utterly infeasible to get to in a short time frame.”
Before the high-powered stimulus of HITECH, the development and refinement of EHRs had been proceeding at an orderly pace. According to Rusty Franz, CEO of NexGen Healthcare, a $500-million-a-year EHR vendor in the physician-office market, “The industry was moving along in a natural Darwinist way, and then along came the stimulus.” He blames the government for its clumsy approach to regulation.“The software got slammed in, and the software wasn’t implemented in a way that supported care,” he said. “It was installed in a way that supported stimulus. My company, we were complicit in it, too.”
Also, not considered in the drafting of the HITECH Act was the fact that healthcare business practices were not aligned with the goal of collaborative exchange of healthcare information. A free exchange of information meant that patients could be treated anywhere. But many healthcare providers are reluctant to lose patients to a competing doctor’s office or hospital. Keeping a tight hold on patients’ medical records was seen as one way to prevent that.
Paving the way for errors
But what worried many doctors most is the ease with which diligent, well-meaning physicians could make serious medical errors. The average ER doctor, for example, will make 4,000 mouse clicks over the course of a shift, and the odds of doing anything 4,000 times without an error is small. Also, physicians tend to see the EHR interfaces as confusing and clunky, thereby making error nearly inevitable.
Glitches at one facility, Mary Rutan Hospital, in Bellefontaine, Ohio, which uses the NexGen software, have included incidents such as the software changing a patient’s gender, seemingly at random, or losing a doctor’s notes on his or her observations after an exam. And NexGen’s maker sometimes took months to address issues.
Dr. Martin Makary, a surgical oncologist at Johns Hopkins and the co-author of a much-cited 2016 study that identified medical errors as the third-leading cause of death in America, credits EHRs for some safety improvements—including recent changes that have helped in curtailing the opioid epidemic. However, technology problems have replaced the historic problems of bad handwriting and missing information.“We’ve swapped one set of problems for another. We used to struggle with handwriting and missing information. We now struggle with a lack of visual cues to know we’re writing and ordering on the correct patient.”
Reducing potential EHR errors
In an accompanying article in this issue of Inside Medical Liability, titled “Electronic Health Record Usability and Patient Safety: Risk and Mitigation Strategies,” Jessica Howe, Zachary Hettinger, and Raj Ratwani of the MedStar Health National Center for Human Factors in Health Care offer recommendations for reducing potential errors.
References
1. Darrel Ranum. Electronic health records continue to lead to medical malpractice suits. The Doctors Company. 2018. https://www.thedoctors.com/articles/electronic-health-records-continue-to-lead-to-medical-malpractice-suits.
2. Darrel Ranum. Electronic health records continue to lead to medical malpractice suits. The Doctors Company. 2018. https://www.thedoctors.com/articles/electronic-health-records-continue-to-lead-to-medical-malpractice-suits.
3. U.S. Department of Health and Human Services. HITECH Act enforcement interim final rule. Feb. 17, 2009, https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html
4. Medical Economics. HIT experts warn about EHR investment in open letter to Obama. Jan. 30, 2009, https://www.medicaleconomics.com/article/hit-experts- warn-about-ehr-investment-open-letter-obama.
5. Darrel Ranum. Electronic health records continue to lead to medical malpractice suits. The Doctors Company. 2018. https://www.thedoctors.com/articles/electronic-health-records-continue-to-lead-to-medical-malpractice-suits.
6. Darrel Ranum. Electronic health records continue to lead to medical malpractice suits. The Doctors Company. 2018. https://www.thedoctors.com/articles/elec- tronic-health-records-continue-to-lead-to-medical-malpractice-suits.
7. Mark L. Graber, et al. Electronic health record-related events in medical malpractice claims. J Pat Saf, June 2019. https://journals.lww.com/journalpatientsafe- ty/Fulltext/2019/06000/Electronic_Health_Record_Related_Events_in_Medical.1. aspx.
8. Mark L. Graber, et al. Electronic health record-related events in medical malpractice claims. J Pat Saf, June 2019. https://journals.lww.com/journalpatientsafe- ty/Fulltext/2019/06000/Electronic_Health_Record_Related_Events_in_Medical.1. aspx.
9. Science Daily. Electronic health records may lower malpractice settlements. Nov. 27, 2008. https://www.sciencedaily.com/releases/2008/11/081125141608.htm.
10. Fred Schulte and Erika Fry. Death by 1,000 clicks: Where electronic health records went wrong. Kaiser Health News. March 18, 2019. https://khn.org/news/death-by-a-thousand-clicks.
11. Fred Schulte and Erika Fry. Death by 1,000 clicks: Where electronic health records went wrong. Kaiser Health News. March 18, 2019. https://khn.org/news/death-by-a-thousand-clicks.
12. Fred Schulte and Erika Fry. Death by 1,000 clicks: Where electronic health records went wrong. Kaiser Health News. March 18, 2019. https://khn.org/news/death-by-a-thousand-clicks.
13. Fred Schulte and Erika Fry. Death by 1,000 clicks: Where electronic health records went wrong. Kaiser Health News. March 18, 2019. https://khn.org/news/death-by-a-thousand-clicks.
14. Fred Schulte and Erika Fry. Death by 1,000 clicks: Where electronic health records went wrong. Kaiser Health News. March 18, 2019. https://khn.org/news/death-by-a-thousand-clicks.