Maternal healthcare is at a critical turning point in the US, as we face some of the highest rates of maternal morbidity and mortality among developed nations. While these issues are challenging, they present a unique opportunity for transformation, offering an exciting opportunity to improve outcomes, enhance patient safety, and reduce costs. Hospitals, health systems, and insurers can make significant strides in maternal care by adopting proactive measures to promote best practices and reduce preventable complications during deliveries.
By implementing a three-step approach, hospitals can optimize obstetric care:
- Identifying areas for improvement in clinical practices
- Discussing potential risks and leveraging data for informed decision-making
- Mitigating complications through targeted interventions and collaboration
One effective strategy is data-driven benchmarking. By analyzing physician practices that lead to malpractice risk and comparing them to regional and national benchmarks, medical professional liability (MPL) insurers and healthcare organizations can identify strengths while uncovering opportunities for improvement. This practice promotes safer environments for expectant mothers, enhancing outcomes, and elevating patient care.
Maternal Care in the United States
With more than 25,000 women experiencing severe maternal complications annually and hundreds of lives lost to maternal causes, there is tremendous potential to drive progress, address existing racial disparities, and enhance the delivery of care.
The American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine recommend identifying potential cases of severe maternal morbidity for further review, focusing on outcomes and complications, and consider this an important step toward promoting safe obstetric care.
Addressing Obstetric Challenges with Innovation
Obstetricians often work long and unpredictable hours to accommodate the unpredictable nature of pregnancy and delivery. Consequently, obstetrics requires a forward-thinking approach to address its complex challenges. Complications such as hemorrhage, hypertension, and preeclampsia are known contributors to adverse outcomes that have increased nearly 200% since 1993. Accounting for roughly 50% of maternal deaths, such complications increase healthcare costs, prolong hospital stays, and lead to significant malpractice claims.
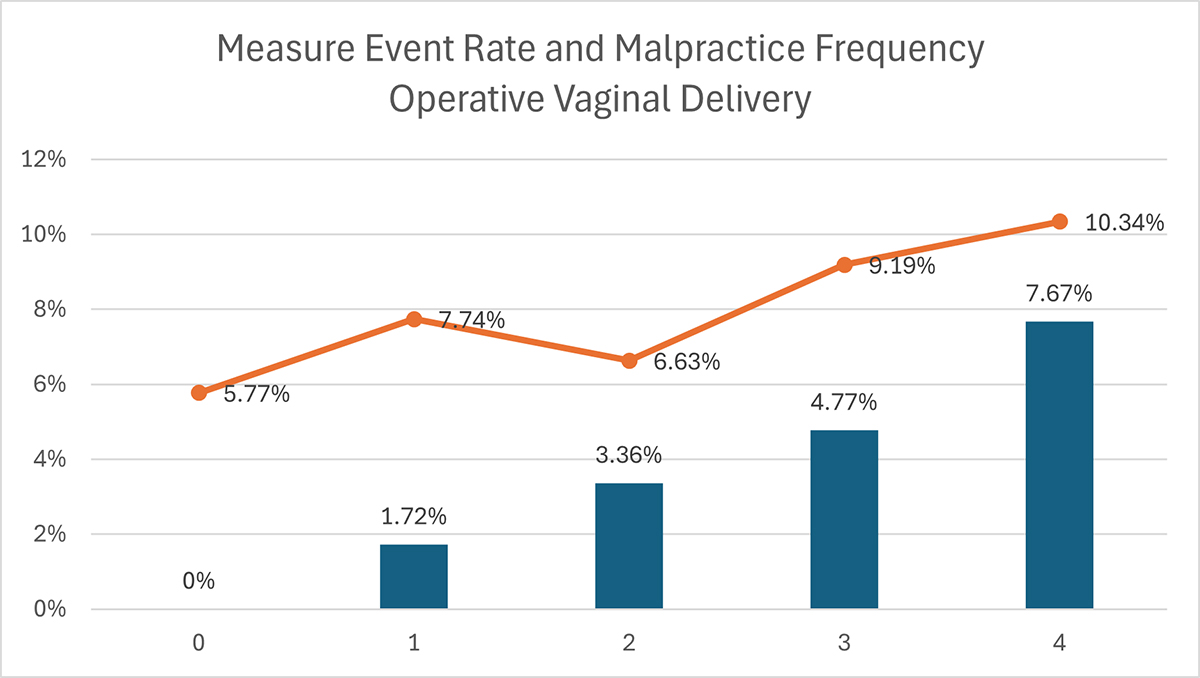
Research consistently demonstrates that adverse birth outcomes, such as birth trauma and severe maternal events, greatly influence the frequency and severity of malpractice claims. For instance, providers with the highest operational vaginal delivery rates are almost twice as likely to face a malpractice claim. Variations in event rates across quartiles reveal notable discrepancies in OB/GYN practice patterns, prompting critical concerns about the risk profiles of certain physicians.
However, these risks can be effectively managed by comparing the outcomes of individual doctors or hospitals with those of similar providers. By examining practice patterns, hospitals and insurers can pinpoint variations in outcomes and develop customized improvement initiatives. For example, data analysis may uncover trends in higher-risk interventions, providing a pathway to mitigate complications through focused support and education for providers. Closing the gaps between outcomes and best practices enables healthcare teams to prevent adverse events and foster safer practices.
Opportunities for Safer Maternal Care
Hospitals and health systems can achieve continuous improvement in obstetric care by addressing variability in outcomes and effectively utilizing data. Care standards can be significantly elevated by tracking performance, reviewing severe maternal morbidity cases, and aligning practices with the latest guidelines established by organizations like the American College of Obstetricians and Gynecologists.

The mantra is simple yet impactful: prioritize harm-free care. Safer maternal care goes far beyond avoiding legal claims; it encompasses transforming lives, building trust, and ensuring a more reliable healthcare system.
Safer Care Through Collaboration
Improving maternal outcomes is not only possible but achievable with the right strategies. We can create a future where safe deliveries and healthy outcomes are the norm by fostering collaboration among physicians, hospitals, and insurers. Emphasizing data, benchmarks, and education provides a roadmap to optimize care while maintaining financial sustainability.
Evidence-Based Approach: With an evidence-based approach, healthcare organizations can leverage actionable insights, foster collaboration, and implement targeted strategies to ensure improved patient outcomes while minimizing risk.
Health systems can begin by understanding their internal metrics on key risk factors, such as complication rates and intervention frequencies. These metrics empower leaders, such as chief medical officers, to guide obstetricians toward meaningful, data-driven improvements in their practice patterns.
Collaboration Through Constructive Dialogue: Clinical and operational leaders can monitor provider performance over time to foster meaningful conversations with individual OB/GYNs. A supportive discussion over a cup of coffee is often enough to inspire a behavior change. This transparent approach encourages accountability, collaboration, and continuous improvement, turning data into positive change.
Actions to Mitigate Risk: Timely reporting aids in risk mitigation. Clinical leaders must be alerted to critical events, such as hemorrhages or unplanned surgical interventions, so they can respond effectively and promptly. Regularly reporting events—within weeks rather than months—helps identify potential issues quickly. Then, leaders should facilitate prompt incident investigations to prevent isolated events from escalating into larger challenges.
Optimizing Outcomes Together
Health systems that implement these data-driven solutions report significant improvements in maternal safety. For example, one major system achieved a 30% reduction in severe maternal complications within three years while simultaneously decreasing MPL claims and reserves related to obstetrics. Leadership teams effectively collaborated to address early warning signs, resulting in measurable improvements in network consistency and patient outcomes.
Improving maternal care is not only possible but also immediately actionable. By leveraging data, fostering collaboration, and taking decisive steps, hospitals can reduce preventable risks, elevate the standard of care, and minimize liability expenses. Together, we can nurture a more consistent and safer future for maternal health.