The frustration of not understanding something, missing a key detail, or assuming someone else will handle it is a familiar human experience. In most industries, the consequences of miscommunication are inconvenience or additional expenses. In medicine, they can be catastrophic, resulting in patient harm, emotional distress, reputational damage, and significant financial loss.
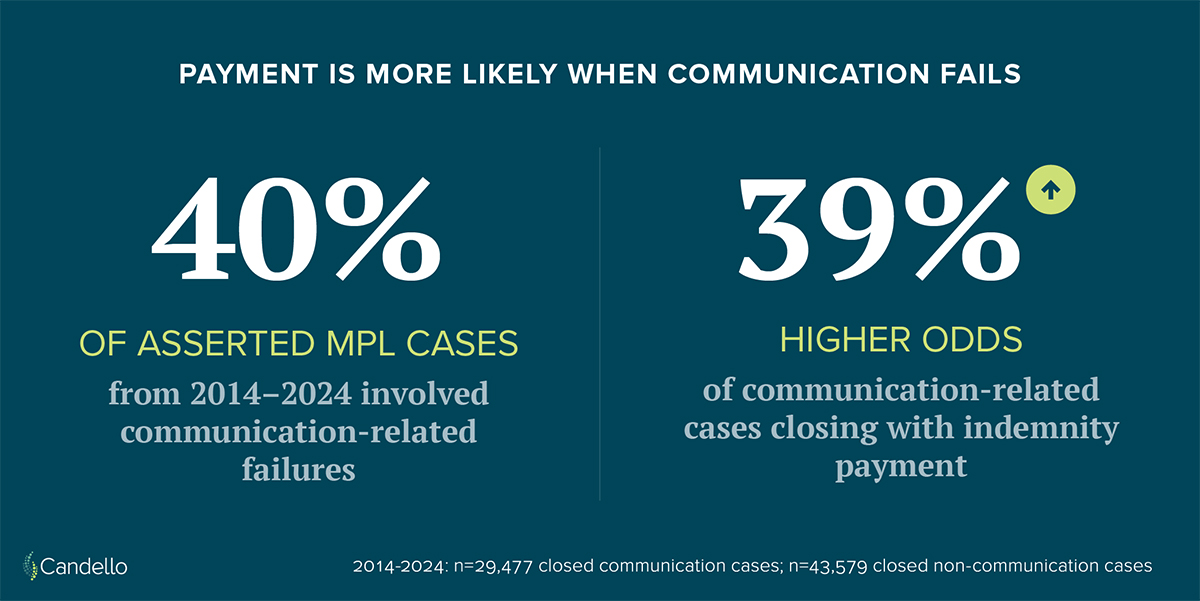
Candello, the claims data collaborative under CRICO, the medical malpractice insurance provider for the Harvard medical community, recently revisited this issue with fresh eyes. In late 2025, Candello analyzed 10 years of closed medical professional liability (MPL) claims involving communication failures and compared the findings with its 2015 Benchmarking Report covering the same topic. The results published in Candello’s report, Malpractice Risks in Communication Failures: A 10-Year Follow Up, should give insurers, healthcare executives, and risk leaders pause. Communication failures are now cited as contributing factors in MPL cases more frequently than a decade ago (40% vs. 31%), and these cases have 39% higher odds of closing with an indemnity payment than cases without communication-related issues.
Communication Failures as a Financial Risk Driver
Medical malpractice claims are rarely caused by a single mistake. They tend to arise from a chain of events, for example, missed test results, unclear handoffs, delayed follow-up, or unrealized conversations. Communication failures often sit at the center of these broken chains.
Evidence from malpractice literature consistently shows that claims involving communication issues are more complex, take longer to resolve, and are more likely to result in payment. Poor communication can obscure clinical reasoning, complicate documentation, and weaken the defensibility of care. When expectations are misaligned or patients feel ignored or misled, dissatisfaction escalates quickly into allegations of negligence.
From a financial standpoint, this matters—and the difference is measurable. During the study period, closed MPL cases involving communication failures had an average indemnity payment of $420,000 and average defense expenses of $79,000. By comparison, closed cases without communication failures had a similar average indemnity payment of $418,000 but notably lower average expenses of $64,000. While the indemnity difference is marginal, the higher associated expenses underscore how communication failures increase claim complexity, prolong resolution, and drive up the total cost of risk beyond the payout itself. Defense expenses, staff time, reputational harm, regulatory scrutiny, and downstream patient attrition all compound the impact.
Provider-Provider vs. Provider-Patient Breakdowns
While communication failures occur across the continuum of care, not all breakdowns carry the same risk profile. Perhaps one of the most concerning findings is the steady rise in communication failures between providers and patients. In the 2015 report, provider-patient communication breakdowns were present in 58% of communication-related cases. In the 2025 analysis, that figure rose to 63%. Additionally, 40% of these cases closed with an indemnity payment averaging $338,000.
Provider-provider communication failures—such as flawed handoffs, incomplete consults, or unclear responsibility for follow-up—remain a major contributor to adverse events. Research on patient safety has repeatedly linked poor handoffs to diagnostic delays, medication errors, and surgical complications. Transitions of care are especially vulnerable moments, where assumptions replace explicit confirmation.
Yet the growth in provider-patient communication failures is especially striking. These failures include inadequate informed consent, unclear explanations of diagnosis or treatment plans, failure to communicate test results, and dismissive or rushed interactions. From a liability perspective, these cases are often harder to defend. Jurors may forgive clinical uncertainty, but they are far less forgiving when patients feel they were not heard or respected.
Why Communication Failures Are Increasing
It is tempting to assume that more technology leads to mean better communication. In reality, the opposite can be true.
Electronic health records have improved access to data but have also fragmented communication. Clinicians may document extensively without ever directly speaking to one another or to the patient. Messages pile up in inboxes, test results auto-release to portals without context, and responsibility becomes diffuse.

Time pressure compounds the problem. Shorter visits, higher patient volumes, and administrative burden leave little room for careful explanation or verification of understanding. Cognitive overload increases the likelihood of assumptions and shortcuts.
Finally, healthcare has grown more complex. Patients often see multiple specialists across multiple settings. Without robust communication structures, gaps are inevitable.
The rise in communication-related claims may reflect not worse intentions, but systems that make failure easier.
Evidence-Based Communication Interventions That Reduce Risk
The good news—for clinicians, patients, and insurers—is that communication failures are highly preventable. Decades of patient safety research point to interventions that meaningfully reduce harm and liability exposure.
Standardized Handoffs: The I-PASS Framework
One of the most studied communication tools in healthcare is I-PASS, a standardized handoff protocol originally developed for inpatient settings. I-PASS stands for Illness severity, Patient summary, Action list, Situation awareness and contingency planning, and Synthesis by receiver.
Large, multi-center studies have shown that implementing I-PASS reduces medical errors and preventable adverse events without increasing handoff time. The tool’s effectiveness also prompted the Agency for Healthcare Research and Quality (AHRQ) to name it the “leading structured handoff tool” in 2025. From a liability perspective, standardized handoffs create shared mental models, reduce ambiguity, and improve documentation quality. For insurers, widespread adoption of structured handoffs represents a tangible risk mitigation strategy.
While I-PASS was designed for inpatient care, its principles translate well to other transitions, including emergency department sign-outs and perioperative handoffs.
Early Disclosure and Communication Programs
Early disclosure programs, sometimes called communication-and-resolution programs (CRPs), encourage transparent, timely communication with patients after adverse events. These programs emphasize acknowledging harm, explaining what is known, apologizing when appropriate, and offering fair compensation without forcing patients into prolonged litigation.
Evidence from health systems that have adopted CRPs suggests that they can reduce the number of claims, shorten resolution time, and lower overall liability costs. Importantly, they also align with patient expectations. Patients consistently report that they want honesty, accountability, empathy, and not silence.
For insurers, early disclosure is not about conceding liability prematurely. It is about reducing the financial and emotional cost of drawn-out disputes fueled by mistrust.
Ambulatory Safety Nets
As more care shifts to outpatient settings, communication risk increasingly lives outside the hospital walls. Ambulatory safety nets are systems designed to ensure that critical information, such as abnormal test results, referrals, and follow-up plans, does not fall through the cracks.
Effective safety nets include clear assignment of responsibility for test result follow-up, closed-loop communication with patients, tracking systems for referrals, and escalation pathways when patients miss appointments or do not respond.
Failures in ambulatory follow-up are a common driver of diagnostic delay claims, which are among the most costly and difficult to defend. Investing in reliable safety nets can significantly reduce exposure in this high-severity category.
Reframing Bedside Manner as a Business Strategy
Improving physician-patient communication is often framed as a professionalism issue. In reality, it is a business imperative.
Research consistently links poor communication to higher malpractice risk, independent of clinical quality. Patients who feel rushed, dismissed, or confused are more likely to sue when outcomes are unfavorable. Conversely, clinicians with strong communication skills tend to face fewer claims, even when complications occur.
Practical interventions include training clinicians to:
- Use plain language and avoid jargon
- Elicit and address patient concerns early
- Confirm understanding using teach-back methods
- Document discussions clearly and contemporaneously
- Acknowledge uncertainty honestly
These behaviors do not require more time so much as more intention. For organizations and insurers, supporting communication skills training is a relatively low-cost intervention with a high potential return.
Implications for Insurers and Healthcare Leaders
The Candello benchmarking data sends a clear message: communication failures are not declining on their own. Left unaddressed, they will continue to drive claim frequency, severity, and indemnity risk.
For medical professional liability insurers, this creates both challenge and opportunity. Premium models, underwriting assessments, and risk management programs should increasingly account for communication practices—not just clinical specialties or historical loss ratios.
For healthcare leaders, communication should be treated as infrastructure. Standardized handoffs, early disclosure programs, ambulatory safety nets, and communication skills training are not optional add-ons. They are core components of a defensible, sustainable care delivery system.
In a complex healthcare environment, miscommunication is expensive. Clarity, by contrast, pays dividends for patients, clinicians, and the organizations that insure them.
As the 2025 Candello analysis makes clear, the financial impact of communication failures is no longer hypothetical. It is measurable, rising, and actionable. The question is not whether organizations can afford to invest in better communication but whether they can afford not to.